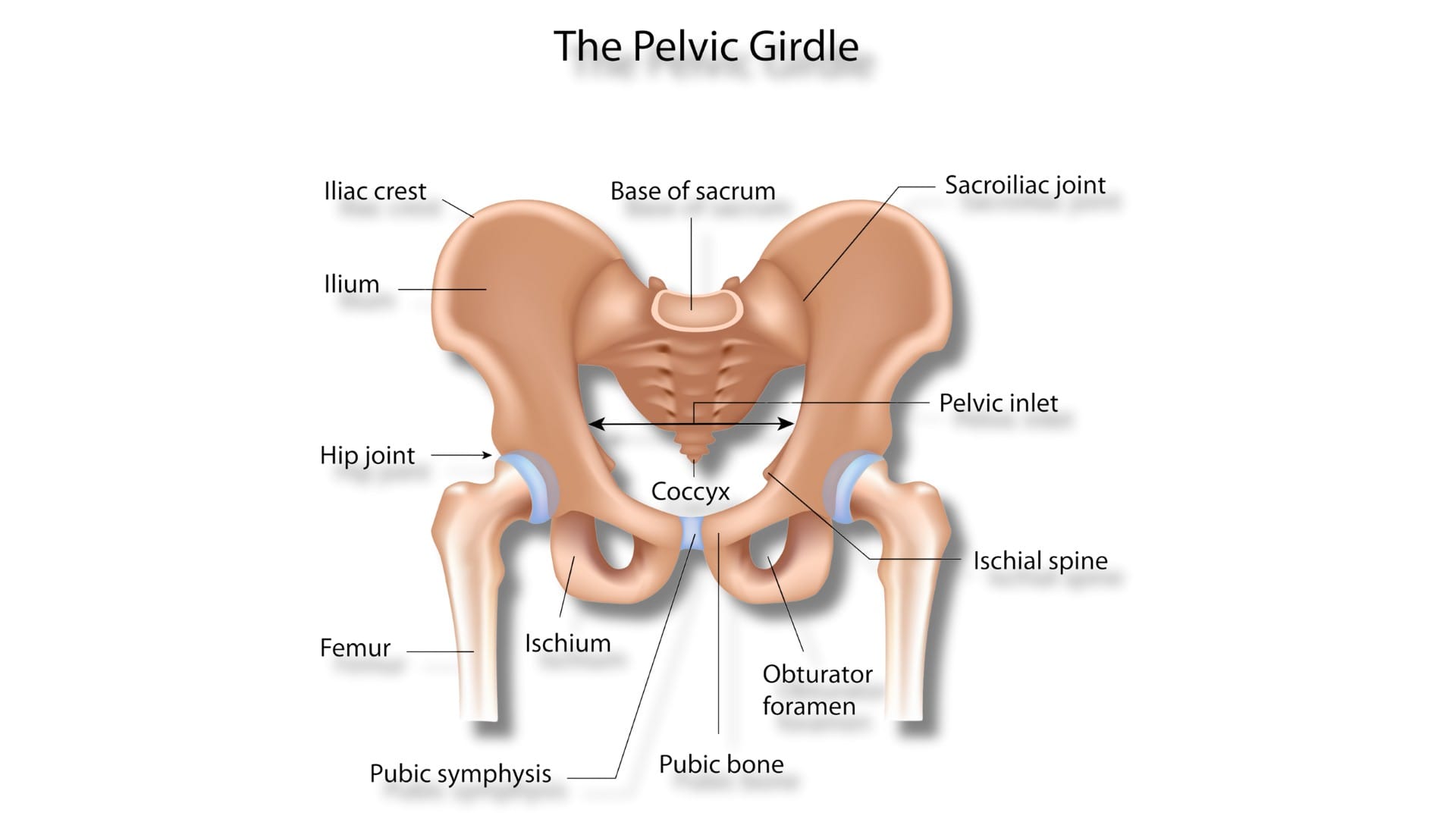
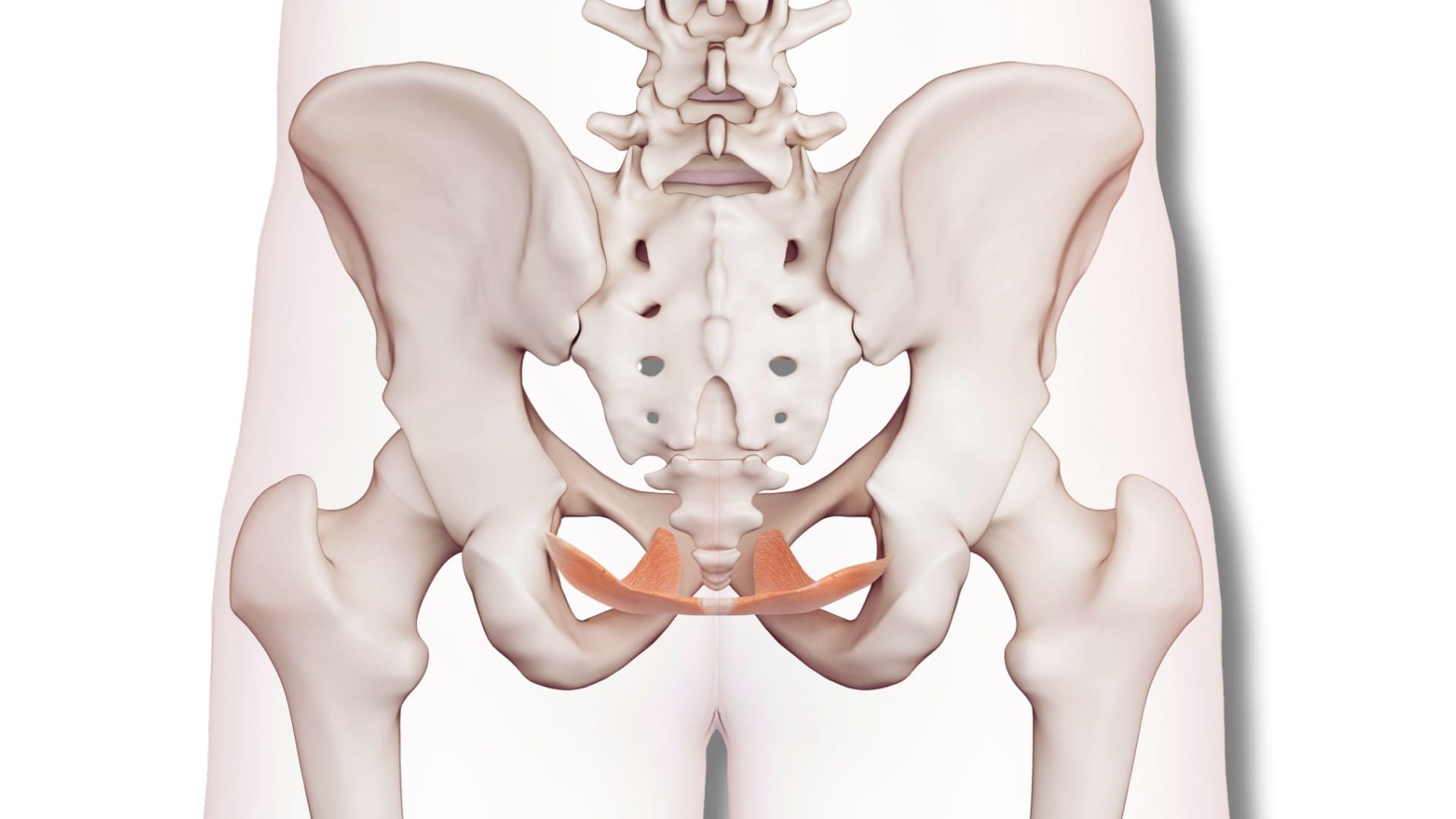
Pelvic floor dysfunction is a functional condition that affects how the muscles, nerves, and connective tissues of the pelvic region work together. The pelvic floor plays a crucial role in everyday bodily functions, including bladder and bowel control, pelvic organ support, sexual function, and core stability. When this system is not functioning in a coordinated way, a variety of symptoms can develop.
For many people, these symptoms appear slowly and may not seem serious at first. Others may notice discomfort but struggle to explain it clearly. Pelvic floor dysfunction can closely resemble urinary, gastrointestinal, or gynecological conditions and is often misunderstood, misdiagnosed, or treated in isolation. A broader, system-based understanding is important to recognize what is really happening and why symptoms persist.
Signs and Symptoms of Pelvic Floor Dysfunction
Pelvic floor dysfunction does not present in a single, uniform way. Symptoms vary depending on muscle tone, nervous system regulation, posture, and individual stress responses. Some people experience mild, occasional symptoms, while others notice persistent issues that interfere with daily life.
- Difficulty starting urination or bowel movements
- Trouble fully emptying the bladder or bowels
- A persistent sensation of incomplete emptying
- Pelvic heaviness, pressure, or a dragging feeling
- Discomfort or pain in the pelvis, lower abdomen, hips, tailbone, or lower back
- Urinary urgency or frequent urination without evidence of infection
- Symptoms that worsen with prolonged sitting, standing, or stress
These symptoms may fluctuate over time, making them easy to ignore or normalize and delaying further evaluation.
Non-Relaxing Pelvic Floor Dysfunction Symptoms
In some individuals, pelvic floor dysfunction is related to muscles that remain overly tense rather than weak. This non-relaxing pattern is often associated with altered neuromuscular signaling and prolonged stress responses.
- Burning, stinging, or discomfort during urination despite normal urine tests
- Constipation that persists despite dietary and lifestyle changes
- Difficulty relaxing during bowel movements
- Pelvic, rectal, or perineal discomfort
- Pain that increases with sitting, prolonged standing, or stress
- A feeling of tightness or pressure deep within the pelvis

Symptoms of Pelvic Floor Dysfunction in Women
Women may experience pelvic floor dysfunction at different stages of life due to hormonal changes, pregnancy, childbirth, pelvic surgery, or menopause. Most common symptoms of pelvic floor dysfunction (PFD) in women:
- Urinary leakage or difficulty controlling urine
- Urinary urgency or frequency
- Pelvic pain, aching, or discomfort
- Difficulty with bowel movements or constipation
- A feeling of pelvic heaviness or pressure
- Pain or discomfort during intimacy
Symptoms may change over time and often overlap with gynecological or urinary conditions, contributing to delayed recognition.

Pelvic Floor Dysfunction in Men: Symptoms and Differences
Pelvic floor dysfunction also affects men, although it is less frequently discussed. Men may experience pelvic, perineal, or rectal discomfort that is difficult to describe clearly. Symptomsof pelvic floor dysfunction in men are:
- Difficulty starting urination
- Incomplete bladder or bowel emptying
- Pelvic pressure or fullness
- Bowel difficulties
- Symptoms are sometimes attributed to prostate-related concerns.
Can Pelvic Floor Dysfunction Feel Like a UTI?
Yes, pelvic floor dysfunction can closely mimic the symptoms of a urinary tract infection. Urinary urgency, frequency, burning, or discomfort may occur even when urine tests show no signs of infection. This similarity often leads to repeated antibiotic treatments that provide little or no lasting relief. When symptoms persist despite normal test results, pelvic floor involvement may be an important factor to consider.
UTI vs Pelvic Floor Dysfunction: How to Tell the Difference
Urinary symptoms such as urgency, frequency, and discomfort are common in both urinary tract infections (UTIs) and pelvic floor dysfunction (PFD). However, the underlying causes, patterns, and management of these conditions differ significantly. UTIs occur when bacteria enter the urinary tract, leading to inflammation and infection. They can affect the bladder (cystitis), kidneys (pyelonephritis), or urethra (urethritis). Symptoms typically develop suddenly and may include:
- Burning sensation during urination (dysuria)
- Frequent and urgent need to urinate
- Cloudy or strong-smelling urine
- Lower abdominal discomfort or pressure
- Occasionally, fever or malaise may occur in more severe infections
UTIs are usually confirmed through laboratory tests, such as urinalysis and urine culture, which identify bacteria and white blood cells in the urine.
| Feature | Urinary Tract Infection (UTI) | Pelvic Floor Dysfunction (PFD) |
| Cause | Bacterial infection of the urinary tract | Muscle coordination and nervous system regulation issues |
| Onset | Sudden, often acute | Gradual or intermittent, may fluctuate |
| Urine Tests | Positive for bacteria, white blood cells | Typically normal, no infection |
| Pain/Discomfort | Burning during urination, lower abdominal pain | Pressure or discomfort in the pelvis, bladder, or perineum |
| Frequency/Urgency | Sudden, constant, infection-driven | May vary with posture, stress, or tension |
| Other Symptoms | Fever, nausea (sometimes), cloudy or strong-smelling urine | Coexisting bowel symptoms, incomplete emptying, tightness or muscle spasm |
| Response to Antibiotics | Typically improves with proper antibiotics | Little or no improvement with antibiotics |
| Assessment Needed | Laboratory urine analysis | Comprehensive pelvic floor evaluation by a trained professional |
| Treatment Approach | Antibiotics, hydration, rest | Pelvic floor exercises, physical therapy, ANF Therapy®, stress, and posture management |
How to Know If You Have a Weak Pelvic Floor?
Pelvic floor dysfunction is not always caused by weakness alone. Some people have reduced muscle strength, others have excessive muscle tension, and many experience a combination of both. As these patterns can coexist, self-testing is often unreliable. Your ANF Therapist will do a detailed assessment to determine the specific pattern involved and create a personalized protocol.

Treatment Options for Pelvic Floor Dysfunction
There are several approaches that may be considered when addressing pelvic floor dysfunction. Management often focuses on improving coordination, reducing excessive muscle tension, and supporting overall pelvic health. These approaches are commonly used individually or in combination, depending on individual needs and professional guidance.
ANF Therapy®
ANF Therapy® is an advanced and non-invasive option for individuals seeking a holistic and supportive approach to pelvic floor dysfunction. This therapy uses small ANF Devices that are applied to specific areas of the body. It is designed to support the body’s natural regulatory and communication processes, particularly those involving the nervous system and muscular coordination. ANF Therapy® does not claim to diagnose or cure pelvic floor dysfunction and is used as a complementary modality within an integrated care plan.
Outcomes
A real-world study involving 1,054 patients across 45 countries evaluated the use of ANF Therapy® in individuals experiencing various musculoskeletal and functional concerns. Results showed a reduction in reported pain levels from an average of 7.6 to 3.1 out of 10 following ANF Therapy® use. Participants also reported reduced swelling and improved range of motion. Overall satisfaction scores were high at 92 out of 100. Mild and short-term effects such as dry mouth, headache, and fatigue were reported by 42 percent of participants. These findings are not specific to pelvic floor dysfunction but reflect broader real-world observations.
Frequently Asked Questions
Is Pelvic Floor Dysfunction Dangerous?
Pelvic floor dysfunction is generally not life-threatening, but it can significantly impact daily comfort and quality of life. If left untreated, it may lead to chronic pelvic pain, urinary urgency, bowel difficulties, and stress, affecting physical and emotional well-being. Early recognition and supportive care can help manage symptoms effectively.
Does Pelvic Floor Dysfunction Cause Hemorrhoids?
PFD doesn’t directly cause hemorrhoids, but poor pelvic floor coordination can increase straining during bowel movements. This extra pressure on rectal veins may worsen existing hemorrhoids or contribute to discomfort. Addressing muscle tension and coordination can reduce this strain.
How Does Pelvic Floor Dysfunction Cause Constipation?
Constipation occurs when pelvic floor muscles fail to relax properly during defecation. Even with a normal diet and bowel habits, stool passage can be difficult, causing straining, incomplete emptying, and discomfort. ANF Therapy®, along with muscle coordination and relaxation strategies, may help restore normal bowel function.
What Happens If Pelvic Floor Dysfunction Goes Untreated?
If left unaddressed, PFD symptoms may persist or worsen over time. Chronic pelvic pain, urinary or bowel difficulties, and discomfort during intimacy or activity can develop. This may reduce daily function, cause stress, and lead to secondary issues like constipation or hemorrhoids.
Pelvic Floor Dysfunction in Women: Why Are Women More Affected?
Women are more prone to PFD due to pregnancy, childbirth, pelvic surgery, and hormonal changes. These factors can weaken or alter pelvic floor muscles, affecting bladder, bowel, and sexual function. Life-stage changes such as menopause may further influence coordination and tissue health.
Conclusion
Pelvic floor dysfunction is a common but often overlooked condition that can affect both women and men. Its symptoms, such as urinary urgency, bowel difficulties, and pelvic discomfort, can be mistaken for infections like UTIs. Early recognition and assessment are important for identifying whether symptoms are due to muscle weakness, tension, or a combination of both. Approaches such as physiotherapy, lifestyle strategies, and complementary support, such as ANF Therapy®, can help improve coordination, reduce tension, and support the body’s natural regulatory processes. Pelvic floor dysfunction needs proactive management to enhance comfort, daily function, and overall quality of life.